Varicose veins are pathological and irreversible changes in the walls of peripheral veins with valve failure and impaired blood flow. Veins of different localization undergo varicose transformation, but most often the vessels of the superficial venous network on the legs are affected, therefore, varicose veins usually mean a disease of the veins of the lower extremities.
How does varicose veins appear?
With varicose veins, only peripheral superficial venous vessels undergo pathological transformation - this is due to the structural features of the walls and the physiology of the outflow of blood from the extremities. It is these pathogenetic moments that are decisive. All other predisposing factors act on the entire vascular system, but do not lead to a characteristic change in the central veins and arteries of any caliber.
Consider the pathogenesis of varicose veins:
- Aseptic inflammation.It starts from the endothelium of the veins and subsequently spreads to the entire thickness of the vessel. The triggering mechanism in most cases is a slowing down of blood flow, there is a parietal grouping of cellular blood elements with leukocyte rolling - a grouping and "rolling" of leukocytes over the surface of the endothelium. Over time, there is a tendency for their adhesion, which provokes the release of inflammatory mediators. At this stage, there are no external changes yet.
- Remodeling of the walls of superficial veins and valves. Leads to a change in density and elasticity. This is facilitated by aseptic inflammation, genetically determined defects in connective tissue proteins, mechanical microdamage to the endothelium, and some other factors. In the affected vessels, the possibilities of reversible compensation of fluctuations in venous pressure are significantly reduced, they become rigid.
- Persistent and progression-prone enlargement of the affected veins.These changes are at first quite local, in the subsequent pathological process spreads not only along the length of one vessel, but also captures other components of the peripheral venous network.
- Compensatory lengthening of the affected vein with the formation of pronounced pathological bends.Characteristic protruding nodes are formed, which gave the name to the disease: "varix" is translated from Latin as "swelling".
- The development of valvular insufficiency.Functional valve failure in the lumen of the affected superficial veins with reverse blood flow (vertical reflux). At first, it has a relative character and manifests itself only with a noticeable increase in peripheral venous pressure. Subsequently, the failure becomes absolute - the walls of the valves do not close completely under any conditions. Venous stasis (blood stasis) appears with the formation of venous insufficiency.
- Involvement of perforating veins in the process.They are also called communicative or commissural. Their pathological expansion is also accompanied by valve insufficiency, which contributes to the pathological blood flow from the deep venous network to the superficial one (horizontal reflux). Increased venous insufficiency.
All these changes are irreversible and persist even with the complete elimination of provoking and predisposing factors, therefore it is impossible to cure already developed varicose veins by conservative methods, it is possible to partially compensate for the violations only for a while.
Causes of varicose veins
Varicose veins is a polyetiological disease, the development is facilitated by external and internal (endogenous) factors. The main reasons for the development of varicose veins:
- Hereditary factor.
- Low mobility, prolonged sitting position.
- In women - changes in hormonal status during pregnancy, taking oral contraceptives, hormone replacement therapy.
- Conditions accompanied by partial compression of the veins of the small pelvis: pregnancy (especially multiple or occurring with polyhydramnios), volumetric formations of the abdominal cavity, some intestinal diseases. Constipation and chronic lung disease with coughing, leading to an increase in intra-abdominal pressure, lead to a violation of venous outflow at the level of the small pelvis.
- Increased body weight.
All people are predisposed to the development of varicose veins. This is due to the vertical position of the body, due to which, under the influence of gravity, the blood tends to the distal parts of the lower extremities, and the veins are under increased stress and are more easily deformed.
Symptoms and manifestations of varicose veins
Symptoms of varicose veins of the superficial thigh and lower leg include:
- Visible changes in the affected veins. Varicose vessels are twisted, overly contoured, dark, translucent through the skin and bulging. Ripple is not peculiar to them. As the disease progresses, local knotty protruding formations appear on the legs, which often form whole conglomerates and do not completely disappear in the supine position. In patients with increased body weight, changes in the veins often remain practically invisible for a long time, masking by excessive subcutaneous fat.
- Swelling of the feet and legs after prolonged standing and sitting, in the evening, when staying in conditions of elevated ambient temperature. Such venous edema is not accompanied by cyanosis of the distal extremities, which can be observed in heart failure. They decrease and even disappear after rest (including a night's sleep), while keeping the legs in an elevated position, after performing special exercises to activate the "muscle pump" of the lower leg. Puffiness is one of the first signs of chronic venous insufficiency with varicose veins.
- Feeling of heaviness and fullness in the legs, even in the absence of obvious edema. Such complaints appear in conditions conducive to pathological blood deposition in the distal parts of the lower extremities. Discomfort is most often noted in the evening and after a long stay in an upright position with little physical activity.
- Signs of muscle ischemia of the limb affected by varicose veins: increased muscle fatigue, sometimes cramps.
- Unpleasant sensations in the legs, usually aggravated by an increase in swelling against the background of the reaction of soft tissues and branches of the peripheral nerves of the lower leg to squeezing by an excessive amount of intercellular fluid. Another possible cause of such paresthesias is dysmetabolic trophic disorders.
- Visible trophic disorders of the skin and underlying soft tissues. These can be dry or eczematous dermatitis, hyperpigmentation, lipodermatosclerosis (compaction, hardening of the dermis and tissue), ulcers.
Symptoms of varicose veins of the lower extremities appear early enough, although not all patients pay attention to them in a timely manner. The order of attaching new features can be different. In some patients, a cosmetic defect in the form of clearly altered veins is initially noted, in others, the disease debuts with the clinic of venous insufficiency.
Stages
The stages of varicose veins are determined according to the CEAP classification:
- C0 - there are no signs of pathology;
- C1 - the presence of reticular varicose veins or telangiectasias;
- C2 - varicose veins;
- C2r - recurrent varicose veins;
- C3 - limb edema;
- C4a - trophic changes: hyperpigmentation or venous eczema;
- C4b - trophic changes in the form of lipodermatosclerosis or white atrophy of the skin;
- С4c - venous crown of the foot;
- C5 - protracted trophic ulcer;
- C6 - open trophic ulcer.
- C6r - recurrent open trophic ulcer.
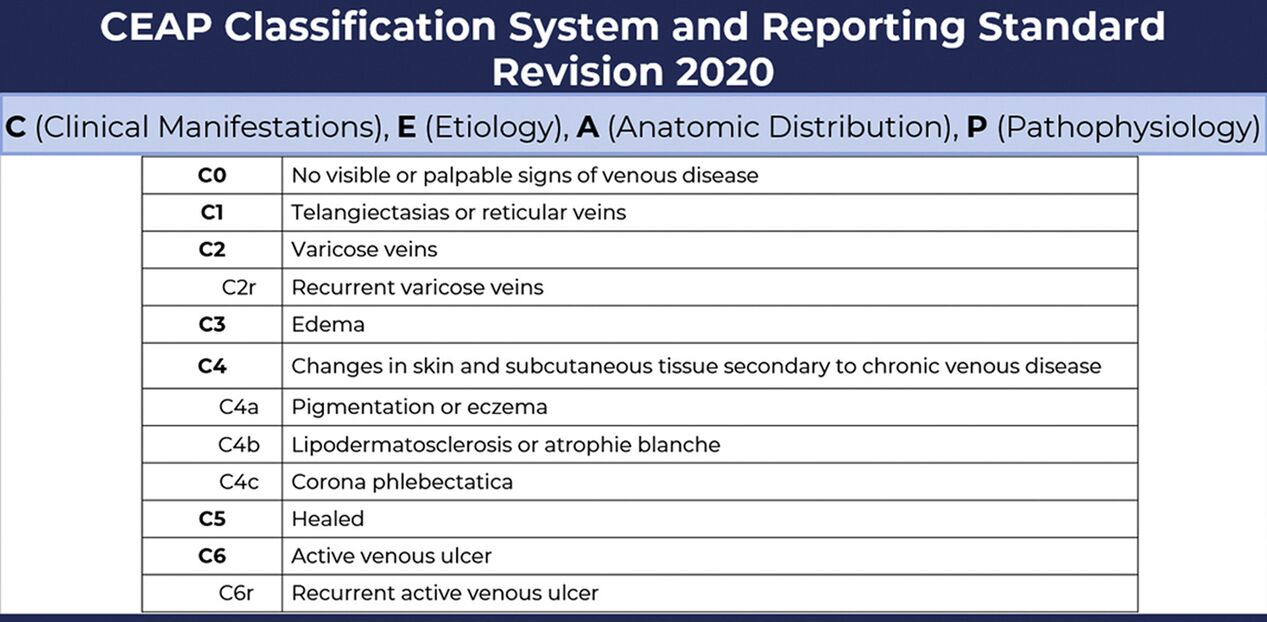
The CEAP classification was created in 1994 and is now internationally accepted. Used by phlebologists when making a diagnosis.
For example, in class C1, only a cosmetic defect is noted - dilated reticular veins of about 1 mm. in diameter, and at C4c it is impossible not to notice serious trophic disturbances.


%20and%20reticular%20veins.jpg)

Diagnostics
A basic examination to confirm the diagnosis of varicose veins of the lower extremities, to clarify the degree and nature of the violations includes:
- Clinical examination. The phlebologist determines the course and condition of visible superficial veins, changes in the skin and soft tissues, the presence of edema. Functional tests are performed to assess vertical reflux and reveal the approximate level of horizontal reflux. Interviewing the patient is aimed at clarifying the predisposing and provoking factors, the duration and features of the development of the disease.
- Ultrasound procedure. With varicose veins, the most informative is not a conventional ultrasound, but an assessment of blood flow using ultrasound (ultrasound). The study shows the speed of blood flow, the presence of pathological veno-venous refluxes, and impaired vascular patency. Such information is necessary for the doctor to select the necessary treatment regimen.
- Hemostasiogram (blood tests for a comprehensive assessment of the coagulation system).

According to the indications, multispiral computed tomography (MS CT) is performed - a high-tech study in some cases becomes the main method for determining the picture of the lesion of the venous system.
In modern medicine, other diagnostic techniques are also used - plethysmography, laser Doppler flowmetry. They are not available to a wide range of patients; the results obtained are usually not critical in determining the treatment tactics. Usually, a basic examination is sufficient, which, if necessary, is supplemented by consultations of narrow specialists (endocrinologist, hematologist, cardiologist and others). Previously, several stages of varicose veins of the legs were distinguished. Currently, when making a diagnosis, phlebologists use the CEAP classification of chronic venous diseases, which includes the characteristics of the case according to clinical, etiological, anatomical and pathophysiological signs.
Danger of varicose veins
Many people think that varicose veins of the lower extremities is mainly a cosmetic problem. Indeed, it is often the external unattractiveness of the legs with knotty bulging blue-violet vessels or vascular network that is the main reason for a visit to the doctor.
Abnormally dilated peripheral veins are a condition that should not be underestimated. It can significantly worsen the patient's well-being and even lead to potentially life-threatening complications. And this is primarily due to the development of chronic venous insufficiency due to persistent and progression-prone hemodynamic disorders. Other unpleasant consequences are also possible.
The consequences of running varicose veins:
- Significant deterioration in the patient's quality of life. Significant discomfort and even a decrease in performance with varicose veins are caused by heavy legs syndrome, edema, nocturnal cramps, poorly healing and recurrent ulcers.
- Changes in soft tissues with a decrease in the external attractiveness of the legs, which is especially important for women. Moreover, hyperpigmentation, lipodermatosclerosis and traces of healed ulcers usually persist even after removal of the affected veins, especially if surgical treatment was carried out against the background of already developed pronounced trophic disorders.
- Bleeding from ruptured varicose veins or veins at the bottom of trophic ulcers.
- Development of thrombosis and thrombophlebitis of superficial veins. It is fraught not only with local hemodynamic disorders and inflammation, but also with distant thromboembolism with heart attacks of various organs and acute life-threatening conditions.
- Deep vein thrombosis is an even more dangerous condition in terms of thromboembolism.
Already developed complications of varicose veins of the thigh and lower leg not only negatively affect the patient's condition and the prognosis of the disease. They significantly reduce the likelihood of getting a quick and sufficient result, even with the use of radical treatment methods.
Is the disease always dangerous?
Varicose veins of the lower extremities with valvular insufficiency of the saphenous veins is not the only possible variant of this pathology. There is also the so-called "cosmetic" variant of varicose veins. According to the classification of chronic venous diseases CEAP is C1, features of the form:
- Lesions of small intradermal vessels up to 3 mm in diameter. They can be subepidermal or reticular.
- The appearance of spider veins, reticular varicose veins in the form of a small superficially located mesh.
- Absence of vertical or horizontal pathological veno-venous reflux. Affected small vessels do not have valves and communicate only with small tributaries of the saphenous veins using the feeding leg. They provide collection of blood from individual sectors of the dermis and its diversion to larger deep-lying vessels. Violation of blood flow at this level does not contribute to the development of chronic venous insufficiency.
This course of the disease does not lead to the development of clinically significant complications. In fact, the patient's discomfort is due to a cosmetic defect. But this does not mean that a person with the presence of spider veins is excluded from the defeat of the veins of a larger caliber. In such a situation, not C1, but C2 and subsequent classes according to the CEAP classification are diagnosed.
Varicose veins treatment
Treatment of varicose veins should not begin with the development of complications, but even at the stage of primary changes and minimally expressed signs of venous insufficiency. One can expect a quick onset of the expected effect, complete regression of symptoms and a low likelihood of relapse. Treatment of advanced varicose veins will not be as effective. Sometimes his task will only be to reduce the rate of progression of the disease, create conditions for the healing of trophic ulcers and reduce the severity of chronic venous insufficiency.
In general, all methods of treating varicose veins of the lower extremities can be divided into non-surgical (conservative) and surgical (radical). Traditionally, most patients prefer sparing techniques, postponing the decision on surgery until the development of complications that cannot be corrected. And many of them do not even go to the doctor, resorting to self-medication. Self-medication often leads to a complication of the pathology.
Conservative treatment
The scheme of conservative treatment of varicose veins includes:
- Systemic drug therapy. It is aimed at improving the rheological properties of blood for the prevention of thrombosis, achieving an anti-inflammatory effect, increasing the elasticity of the vascular wall, and stimulating tissue regeneration.
- Local drug therapy (ointments, creams, gels). External remedies are designed to improve microcirculation, reduce puffiness, increase venous tone, and heal trophic ulcers.
- Physiotherapy exercises increase the efficiency of the lower leg muscle pump and thereby improve blood flow from the legs.
- Use of compression hosiery. Compression stockings, pantyhose exert dosed compression of superficially located veins, which reduces the tendency to deposit blood and edema, improves well-being, and reduces the likelihood of thrombosis.
- Physiotherapy. They are used mainly in the absence of open trophic ulcers and outside the acute stage of thrombophlebitis. Applied hardware pneumocompression, darsonvalization, galvanization, UHF therapy, UV therapy, hydrotherapy, ozone therapy. The tasks of physiotherapy include improving venous and lymphatic outflow, improving microcirculation, stimulating regeneration, and reducing the severity of discomfort.

Medicines will not return healthy blood flow to the already changed veins, they will remain convoluted and dilated. And even a slight increase in the tone of the vascular wall under the action of phlebotonics will not be able to completely correct the valve insufficiency.
You should not expect high results from conservative treatment. It will reduce pain and the severity of edema, reduce the risk of thrombosis and improve the healing of trophic disorders. But it is impossible to save the patient from varicose veins and prevent further progression of the disease with a conservative approach.
Surgery
An invasive (surgical) method of treating varicose veins is aimed at turning off the affected vessel and its main tributaries from the general bloodstream (by removing or obliterating it) and eliminating horizontal veno-venous reflux. Does not aggravate tissue ischemia, improves trophism by significantly reducing (or even eliminating) venous stasis. Such treatment not only removes the cosmetic defect, but also helps to cope with chronic venous insufficiency.
Classic surgical methods for treating varicose veins of the lower extremities:
- Crossectomy is a complete transection of a ligated large superficial vein at the place of its confluence with the deep venous network.
- Phlebectomy - removal of the superficial vein affected by varicose veins (large or small saphenous vein). It is produced by stripping (pulling, pulling out) the vessel with instruments through small incisions. Currently, it is combined with crossectomy and removal of tributaries.
- Miniflebectomy - removal of large perforators and tributaries through small incisions or punctures.
For a long time, the main method of surgical treatment was open surgery, their disadvantages:
- Perceptible blood loss;
- Hemorrhages in the area of the operation, sometimes requiring reoperation to evacuate blood.
- Lymphostasis due to the intersection of lymphatic vessels.
- Severe pain syndrome.
- Long-term disability.
Modern alternative to surgery
Endovascular techniques are referred to as minimally invasive interventions; they do not require incisions. They are not so traumatic, in terms of effectiveness they are not inferior to classical operations. Complications and relapses after them are less common than after operations.
Minimally invasive methods:
- Laser obliteration
- Sclerotherapy / Cryosclerotherapy
- Radiofrequency obliteration.
With minimally invasive methods, the varicose vein is not removed, as with classical operations. Its wall is exposed to laser or radiofrequency energy from the inside, and during sclerotherapy - a sclerosant drug. This provokes "sticking" of the vessel and its subsequent fibrosis, replacement by connective tissue. This closure of the vessel lumen is called obliteration. And with the RFO of the stars, they are actually evaporated by the action of radio frequency waves.






























